Defining Controlled Substances Overdose: ...
Source: United Nations Office on Drugs and Crime
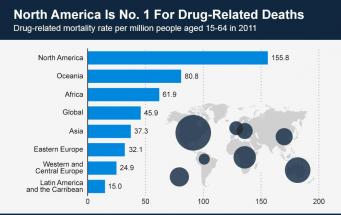
Current Trends in Drug Abuse
United States Drug Use Trends and Statistics
Overdose Mortality Data
Harm Reduction
Overdose Prevention
Overview
Originally Published: 08/08/2013
Post Date: 08/08/2013
by Nabarun Dasgupta, Scott Proescholdbell, Catherine Sanford, et al.
Attachment Files
Summary/Abstract
The rate of mortality attributable to drug poisoning has risen consistently since the 1990s. State-based vital statistics registries estimate the incidence of drug overdose deaths using International Classification of Disease 10th revision (ICD-10) codes. Composite ICD-10-based definitions of “overdose” may include deaths that do not involve controlled substances while missing deaths that do. This has implications for incidence estimates, funding priorities, and intervention evaluation.
Content
Defining Controlled Substances Overdose: Should Deaths from Substance use Disorders and Pharmaceutical Adverse Events be included?
| Abbreviations | |
| ACE: Angiotensin-converting-enzyme; COPD: Chronic Obstructive Pulmonary Disease; CFR: Code of Federal Regulations; CDC: Centers for Disease Control and Prevention; FDA: Food and Drug Administration; ISW: Injury Surveillance Workgroup; ICD-10: International Classification of Disease 10th revision; IQR: Interquartile Range; NCHS: National Center for Health Statistics; NCIP: National Center for Injury Prevention and Control; NCP: North Carolina | |
| Introduction | |
| In the United States, the rate of mortality attributable to drug poisonings has risen consistently since the early 1990s [1,2]. In 2008, the national age-adjusted death rate from drug poisonings was 11.9 per 100,000, making it the leading cause of injury death, surpassing motor vehicle-related fatalities [3]. Drug poisoning mortality outpaces injection-borne infectious diseases, including HIV and viral hepatitis, as the leading cause of death among young injection drug users in the United States [4]. | |
| Since 1999, national mortality data have been coded using the International Classification of Disease 10th Revision (ICD-10) maintained by the World Health Organization. Using ICD-10, each death is assigned a single underlying cause and up to 20 contributing causes. To compute incidence estimates for poisonings, death certificate data and medical examiner case records are tabulated in state and territorial vital statistics systems, and reported nationally through the National Vital Statistics System of the National Center for Health Statistics (NCHS) for the Centers for Disease Control and Prevention (CDC). | |
| There is considerable interest in the timely and accurate identification of deaths from ingesting psychotropic (controlled) substances in amounts that directly cause or contribute to a fatality (consistent with the US Food and Drug Administration (FDA) definition of a serious adverse event;21 CFR § 314.80). For controlled substances the most relevant ICD-10 codes are: poisoning by narcotics and hallucinogens (X42, X60 and Y12; unintentional, intentional and undetermined intent, respectively); and three codes (X41, X61, Y11) that include other controlled substances, such as sedatives and other psychotropic drugs, as well as less frequently prescribed non-controlled medicines for epilepsy and Parkinson’s disease that are dopaminergic precursors or otherwise increase dopamine activity. We collectively refer to these codes (X42, X60, Y12, X41, X61, Y11) as "poisonings from controlled substances." | |
| The National Center for Injury Prevention and Control (NCIP) and NCHS identify drug poisoning deaths only using X- and Y- chapter poisoning codes (Table 1) [5]. However, there is concern that using these codes alone may underestimate overdose deaths in surveillance data [6,7]. The multi-disciplinary Injury Surveillance Workgroup (ISW) of the Safe States Alliance recently suggested five possible consensusbased recommendations of ICD codes to be used for identifying overdose events, based on more expansive definitions that include substance use disorder and a wide list of pharmaceutical adverse event codes [8,9]. However the inclusion of non-controlled medicines in the definition may overestimate overdose events. | |
| We evaluated definitional issues of using ICD-10 codes for drug overdose death surveillance in a two-step process. First, we assessed the effect of including substance use disorder codes with the goal of implementing a more inclusive ("broad") definition of drug overdose involving controlled substances. Second, we evaluated the effect of excluding deaths due to pharmaceutical adverse events in "broad" surveillance definitions for drug overdose involving controlled substances. | |
| All of the NCHS and ISW definitions (Table 1) include deaths from pharmaceutical adverse events, even if the medicines involved were not controlled substances [9-11]. We could not find a clear justification for this. The FDA has used some of these exact codes to identify adverse event deaths unrelated to controlled substances, for example when reviewing the risk of infection associated with corticosteroid treatment [12,13]. Discrepancies such as these between federal health agencies necessitate a closer look at the definitions of overdose. This study explored which pharmaceutical adverse event death should be included in definitions of overdose mortality for controlled substances. This topic is of significance worldwide, for surveillance and incidence estimates and for researchers seeking to evaluate interventions to prevent overdoses from controlled substances. | |
| We applied seven ICD-10 based definitions of "drug poisoning" or "overdose" to four years of mortality data from North Carolina (NC). NC vital statistics data are collected in a statewide electronic medical examiner records system overseen by the North Carolina Office of the Chief Medical Examiner [7]. | |
| Methods | |
| The study population was any NC resident whose death was recorded in NC vital statistics as having occurred from January 1, 2008 through December 31, 2011. | |
| Mortality data source | |
| Each death triggers a registration of the death with a local or municipal health authority, a mandated administrative task. The causeof- death is determined by local health directors, attending physicians, or medical examiners based on autopsies or other investigations. Once the cause(s) of death are determined, the death record is appended, i.e., with the literal words used to describe the cause of death, which may occur months after the issuance of the original certification of death. The death records are converted by individual nosologists or computer software to alphanumeric ICD-10codes. Mortality data for 2008 through 2010 were obtained from the North Carolina Vital Statistics Dataverse at The Howard W. Odum Institute for Social Science of the University of North Carolina at Chapel Hill [14]. Vital statistics mortality data for 2011 were obtained from the Injury and Violence Prevention Branch, North Carolina Division of Public Health, Department of Health and Human Services, as were death certificate data listing the literal text of the cause-of-death fields for 2010 and 2011. | |
| Definitions | |
| We analyzed one definition of overdose used by NCHS, five consensus-based definitions proposed by ISW, and one used for surveillance of opioid-related mortality by public health authorities in Australia [8] (Table 1). Definitions 1, 2, and 3 are intended to broadly identify all overdoses due to "drugs" and controlled substances. Definitions 4, 5, and 7 are intended to specifically identify opioid overdoses; whereas Definition 6 only identifies prescription opioid overdoses. All seven definitions include the aforementioned six codes for poisonings from controlled substances. All definitions include homicidal poisoning using drugs or biological substances (X85).The definitions can also include deaths due to substance use disorders (Definitions 2, 3, 4, 7),pharmaceutical adverse events (all), the involvement of heroin (all except Definition 6), cocaine and other drugs (Definitions 1, 2, 3),or unspecified narcotics (all except Definition 6). | |
| Substance use disorder codes are found in chapter F of ICD-10, with the following two-digit number indicating the substance, e.g., opioids are F11. A fourth digit suffix indicates the chronicity of substance use that led to the death. The codes of greatest relevance for mortality are: acute intoxication (.0), harmful use (.1), dependence syndrome (.2), withdrawal (.3), and unspecified chronicity (.9). The presence of an acute intoxication code (e.g., F11.0 for opioids) is in conflict with unintentional poisoning code (e.g., X42 for opioids). Accordingly, in 2007 NCHS discontinued the use of acute intoxication F codes for underlying cause-of-death in favor of X- and Y- chapter poisoning codes [9] (this convention may have continued at the state level beyond 2007). However, substance use disorder codes of other chronicity (e.g., not .1) continued to be used. | |
| Among the seven definitions, pharmaceutical adverse events were identified using three approaches, the first of which uses poisoning codes as underlying causes (X40, X43, X44, X60, X63, X64, Y10, Y13, Y14). This results in Definitions 1 through 6 including deaths from controlled substances and non-controlled medicines. Some of these are: non-opioid analgesics, fever reducers (aspirin), tumor necrosis factor inhibitors, acetylcholine, albuterol, atropine, propanol, and ergotamine, as well as "other and unspecified drugs that act on the autonomic nervous system or elsewhere." We collectively refer to these as "poisonings from other and unknown substances." | |
| In the second approach, Definitions 2 and 4 also include deaths with an underlying cause in the range of Y40 through Y59, which are poisonings resulting from medicines causing adverse events during therapeutic use, i.e., iatrogenic exposures. Medicines could include: anti-coagulants, antibiotics, bacterial vaccines, immunosuppressive agents, Angiotensin-Converting-Enzyme (ACE) inhibitors, and others. Of particular interest is Y45.0 which designates deaths due to the use of opioids and related analgesics during therapeutic use. The third way to identify adverse events is by using outcomes codes that suggest physiologic harm. ISW constructed Definitions 2 and 4to include 34 specific drug-induced underlying causes including medicine-induced versions of conditions such as aplastic anemia, pancreatitis, gout, obesity, osteoporosis, and lupus erythematous, traditionally used for pharmaceutical adverse event reporting. We collectively refer to these as "adverse events during therapeutic use." | |
| The Australian surveillance definition (Definition 7) uses a different approach to specifically identify opioid overdose deaths (Table 1). It includes deaths due to any underlying cause that is opioid related, defined as the presence of any of the following in contributing cause-of-death fields: T40.0, T40.1, T40.2, T40.3, T40.4, T40.6, or F11 [8]. For example, Definition 7 includes deaths with underlying causes for asthma or chronic obstructive pulmonary disease (COPD) that also have contributing causes that show opioid toxicity. None of the other definitions include these cases but they are likely cases of interest to us. | |
| To examine the involvement of multiple controlled substances in overdose deaths, we defined controlled substance toxicology collectively as the following ICD-10 codes: opioids (T40.0, T40.1, T40.2, T40.3, T40.4), cocaine (T40.5), "narcotic" unspecified (T40.6), benzodiazepines (T42.4), amphetamine-type stimulants (T43.6), ketamine (T41.2), cannabis (T40.7), hallucinogens (T40.8, T40.9), barbiturates (T42.3) and gamma hydroxybutyrate (T52.8). Ethanol toxicity (T51.0) was considered separately. The intent of the ICD- 10 schema is that these codes are not intended to represent the mere presence of the substance in post-mortem toxicology findings or circumstantial evidence, but rather indicate their causal involvement in the fatality. | |
| Statistical analysis | |
| We compared seven definitions to each other using bivariate and descriptive statistics, with particular attention to Definition 1 because it is used by NCHS. Variables of interest included: sex, race and ethnicity, age, marital status, whether an autopsy was conducted, and place of death. Sex differences were examined because differences in opioid effects have been documented in clinical trials [15,16]. Age and racial differences have been observed in opioid metabolism [17,18] and dependence [19]. We also compared definitions on whether the death was intentional, unintentional or of undetermined intent. Previous analyses have noted empirical interstate variation in the classification of intent of overdose deaths [20] and we explored whether variations within a state could also be ascertained. All data analysis was conducted in STATA 12 (College Station, Texas). Population rates were calculated using Poisson regression with population denominators from NCHS bridged population estimates. | |
| Human subjects protections | |
| This research was reviewed by the University of North Carolina Non-Biomedical Institutional Review Board and deemed to be exempt according to federal standards because mortality data were de-identified and publicly available. | |
| Results | |
| Describing drug overdose deaths | |
| There were 322,458 deaths recorded in vital statistics for North Carolina from January 1, 2008 through December 31, 2011. Of these, 312,287 deaths were among North Carolina residents, after removing two decedents for whom exact dates of death were missing. Among the resulting records, 4,898 deaths (1.5%) fit at least one of the seven definitions during the four-year study period. Definition 1 used by NCHS and Definition 3 proposed by ISW identified exactly the same deaths (Table 2). | |
| Annual drug poisoning mortality rates among North Carolina residents were 12.7 per 100,000 residents in 2008, 12.3 in 2009, 11.2 in 2010, and 12.6 in 2011, using Definition 1 or 3. Nearly all deaths were certified by medical examiners (95.8%) or physicians (3.4%), with 37occurring outside of NC certified by coroners. Autopsies were performed in 76.6% to 88.4% of cases depending on the definition, with the prescription opioid-specific definitions (Definitions 4 through 7) more likely to have had an autopsy performed. By comparison, 7.2% of all deaths among NC residents had an autopsy performed. | |
| The seven mortality definitions shared common demographic characteristics. The sex distribution showed minor variation, ranging from 38% female in the most opioid-specific definitions to 41% for the broader ones (Table 3). The racial and ethnic distribution of decedents meeting Definition 1 or 3 was non-Hispanic white (89.0%) or black (8.0%), Native American (1.8%), any race Hispanic (0.9%), and other races and ethnicities (0.3%). The opioid-specific definitions had a slightly higher percent of white non-Hispanic decedents, for example 92.5% in Definition 5. Marital status at time of death was known for 99.5% of decedents included in Definition 1 or 3. One-third of the decedents never married, one-third were married at the time of death, and a quarter was divorced. The age distributions generally had a smaller peak in the mid-to-late 20s, a second greater peak in the middle-to-late 40s and rapid decline thereafter. | |
| The seven definitions had similar proportions of intentional, unintentional, and intent-unspecified deaths. As an example, Definition 1 or 3 had 3,761 (81.1%) that were unintentional, 694 (15.0%) that were intentional or suicides, and 178 (3.8%) of undetermined intent. Only two deaths from poisoning homicide with controlled substances were identified, both in children. | |
| Prescription opioids were involved in 61% to 63% of all drug overdose deaths identified using Definitions 1, 2, and 3, Table 3. When reviewing definitions restricted to opioids (definitions 4 through 7) in North Carolina, prescription opioids were involved in 90% to 91% of all deaths involving opioids, whereas heroin was identified in 7.7% to 7.9% of all deaths involving opioids. Cocaine was implicated in 8.5% to 9.7% of the opioid-specific deaths (Definitions 4 through 7). | |
| Definition 2 identified the greatest number of overdose deaths. However, definition 7 identified the greatest number of opioid overdose deaths since it could include any underlying cause-of-death, Table 3. The two broadest ISW Definitions 4 and 5 only differed by 12 deaths since they take the same approach of relying on toxicity codes in contributing cause fields for the identification of opioid deaths. For the sake of brevity the former was not considered in subsequent analysis. | |
| Identifying pharmaceutical adverse event and substance use disorder codes | |
| Since we were concerned about a potential underestimate of overdose deaths, we focused our attention on the two definitions that identified the most cases, Definition 2 for all drugs and Definition 7 for opioid-related deaths. Definition 2 included4, 807 (annual average: 1,202) deaths during four years, representing a 3.7% increase over the 4,635 deaths (annual average: 1,159) identified with Definition 1 or 3, Figure 1. Poisonings due to controlled substances made up 68.6% (n=3,299) of drug overdose deaths identified using Definition 2 (Table 4 and white circle in Figure 1). However 1,334 poisoning deaths from other and unknown substances make it difficult to understand which substances were implicated. Deaths in this category were of interest because theoretically some could have been excluded since they are pharmaceutical adverse events not involving controlled substances. The underlying cause-of-death field provides little additional information; 94% were due to a trio of codes for "poisoning by other and unspecified drugs, medicaments and biological substances": X44(n=887), X64 (n=303), and Y14 (n=69), of unintentional, intentional, and undetermined intent, respectively. However, the contributing causeof- death fields provided additional information to characterize these deaths. Despite an underlying cause-of-death that suggested that the substance involved was unknown, 586of the 1,334 deaths had controlled substance toxicity codes as contributing causes (Figure 1): opioids (n=553), cocaine (n=369), benzodiazepines (n=86), and amphetamine-type stimulants (n=24), with more than one controlled substance toxicity code in 362 records. Of the remaining 748 deaths, the only toxicology code listed for 52.5% (n=393)records was "unspecified drugs, acidifying agents, alkalizing agents, immunoglobulin, parathyroid hormones" (T50.9).Among the remaining 355 deaths, 61 had codes for disorders due to the use of multiple substances (e.g., F19). That left 294 deaths that had toxicology codes for a variety of medicines that had no evidence of involving controlled substances: anti-allergic and antiemetic drugs, acetaminophen, respiratory system agents, nonsteroidal anti-inflammatory drugs, insulin and oral diabetes medicines, aspirin, anti-coagulants, calcium-channel blockers, cardiac-stimulant glycosides and anti-dysrhythmic drugs, and anti-depressants, Figure 1. These do not appear to be deaths of interest for this analysis. | |
| Another way to assess the contribution of pharmaceutical adverse events is by comparing the 172 additional overdose deaths identified using Definition 2 versus Definitions 1or 3 (Figure 1, grey penumbra). This also provides insight into the importance of including substance use disorder codes. Among the 172 deaths there were 112 with substance use disorder underlying causes (F11 to F19), including sedatives, cocaine, amphetamine-type stimulants, and multiple drugs (Figure 1, right box). The F codes were used in deaths statewide and do not appear to be an artifact of isolated individual medical examiner conventions. The median age of decedents with substance use disorder codes was 50.0 years (IQR: 42.5, 58), compared to 42years (IQR: 31, 50) for poisonings from controlled substances, Table 4. Other demographic characteristics were similar between deaths identified using the substance use disorder and poisonings from controlled substances codes. | |
| Of the remaining 60 deaths, 58 deaths were caused by adverse events involving medicines in therapeutic use (Y40 throughY59) (Figure 1, right box). Only two deaths were due to controlled substances, specifically opioids during therapeutic use (Y45.0). As a group, the deaths involving adverse events during therapeutic use were older (median 65.5 years, IQR: 48, 77.5) than substance use disorder deaths or poisonings from controlled substances, Table 4, and may not be a death from an overdose of the type in which we are interested. | |
| Two remaining deaths due to pharmaceutical adverse events were identified using Definition 2 proposed by ISW one from drug-induced secondary Parkinsonism (G21.1) and one death from drug-induced myopathy (G72.0). These two deaths also do not appear to be of interest in this analysis, as there were multiple co-morbid conditions and both deaths were among 70-year-olds. | |
| Expanding the Definition | |
| We also explored whether the approach in Definition 7 of including deaths with controlled substance poisoning and toxicology codes in contributing cause-of-death fields would change the number of drug overdose deaths identified. Including deaths with any underlying cause that have contributing causes among the six controlled substance poisoning codes (X41, X42, X61, X62, Y11, Y12) adds 108 deaths not identified by Definition 2, Figure 1.Similarly, Definition 2 did not include 126 deaths where controlled substance toxicology codes were present. There was an overlap of 90 deaths between these two approaches, so a total of 145 additional deaths were identified that may be drug overdoses from controlled substances, Figure 1. The most common underlying causes were circulatory system disorders, such as non-congestive heart failure. | |
| There were 145 overdose deaths involving controlled substances that were not identified using either the NCHS or ISW definitions, Figure 1. These deaths were identified by allowing records with any underlying cause with at least one contributing cause from among the controlled substance poisoning or toxicity codes. For example, the death of a 32-year-old male had an underlying cause of pneumonitis from aspirated vomit, but was accompanied by a controlled substance poisoning X code, adult respiratory distress syndrome, and opioid, benzodiazepine and cocaine toxicity codes. These deaths should be considered for inclusion in overdose definitions for controlled substances (Table 5). | |
| Discussion | |
| Our intent was to identify deaths that were the result of ingesting controlled substances in amounts that directly cause or contribute to a fatality. We hypothesized that ICD-10-based definitions of overdose mortality may include deaths that do not involve controlled substances while simultaneously missing deaths that do. Our findings suggest that this is likely the case. | |
| In the North Carolina data over four years, 6.3% (n=294) of the deaths identified using the NCHS definition (n=4,635) were pharmaceutical adverse events where non-controlled medicines were indicated via toxicology codes, and there was no mention of involvement of any controlled substance. If the 393 poisoning deaths from unknown substances were actually due to non-controlled substances, it would be 14.8%. Using Definition 2 and including the 58 pharmaceutical adverse events, as many as 15.5% of deaths for "overdose" may not involve controlled substances. Similarly, including poisonings of medicines with therapeutic intent (Y40 through Y59) did not pick up additional deaths of interest, and these decedents were older than deaths identified using poisoning or substance use disorder codes. There appears to be no direct benefit of adding these deaths to surveillance definitions that are focused on controlled substances, although they may by relevant to pharmacovigilance and adverse event reporting [11,21,22]. Finally, including the drug-induced somatic codes proposed by ISW resulted in a couple of additional cases that did not appear to involve controlled substances. | |
| Proposed Definition | |
| We propose a refined definition that borrows upon the work of NCHS, ISW and the Australians (Definition 8, Table 5). Conceptually starting with the definition that identified the greatest number of records (Definition 2 from the ISW) our proposed definition removes 354 deaths that were due to pharmaceutical adverse events and homicide, and adds 145 deaths not previously identified, yielding 4,598 overdose deaths involving controlled substances during four years, indicated in Figure 1with asterisks. The total number of deaths among NC residents over four years identified using the NCHS definition (Definition 1) (n=4,635) and our proposed definition (n=4,598) differ only slightly. | |
| In addition to the three broad definitions for overdose deaths from controlled substances, we evaluated four opioid-specific ones (including three proposed by ISW) for the sake of completeness and because deaths involving opioids have become a major public health concern [2]. Also, we borrowed concepts from Definition 7 described by Jauncey and colleagues (2005) in proposing our own definition. | |
| The ICD defines T50.9 as a catchall for medical products not explicitly mentioned in the coding schema, including medicines acting on the cardiovascular and gastro-intestinal system, hormones, antibiotics, vaccines, and topical preparations, to name a few. The choice to include the 393 records in our proposed definition can be called into question, as there may be a desire by some to only attribute events to controlled substances where a specific psychotropic drug is identified(e.g., positive evidence).While we acknowledge that this code may result in including deaths from non-controlled substances, given the lack of standardization of assays, autopsy, and coding practices, the absence of negative evidence implores us to consider these deaths in the definition. One practical solution would be to conduct a sensitivity analysis with and without the T50.9-only poisonings deaths, and present both results. In our study, the number of overdose deaths would accordingly range from 4,205 to 4,598, a change of less than 100 deaths per year. | |
| We entertained the possibility of including deaths with controlled substance use disorder codes in contributing cause fields. While there were some deaths that could possibly have been due to overdose, the most common underlying causes of death included chronic harms of injection drug use, such as viral hepatitis and HIV. In some of these instances the last exposure to the substance may have been days, or even decades, ago. It is possible that our proposed definition is also an underestimate of the actual overdose deaths from controlled substances. | |
| In the absence of a gold standard against which to compare definitions of overdose deaths using vital statistics we have chosen to focus on internal validity. This is the primary limitation of our analysis. We anticipate that the availability of electronic health records and medical examiner systems will allow us to compare overdose deaths identified in vital statistics with those identified using medical records in the future, extending analyses of others [23]. | |
| It is possible that not all deaths determined to be overdoses by medical examiners are accordingly identified [24,25]. To address this concern, qualitative and quantitative methods that include interviews with active drug users, overdose survivors and family members of decedents can be used [26-30]. It may also be important to differentiate instances where illicitly manufactured drugs may contain contaminants that are the primary cause-of-death, and the controlled substance is in low concentration. Further work is needed to uncover what convention coding practices are under this scenario. | |
| Conclusion | |
| Overdose deaths from controlled substances present a serious public health problem and accurate estimates of the numbers of such deaths are critical to ongoing public health surveillance. State health department injury control officials should carefully choose which ICD- 10 codes are most relevant for their state. We feel that deaths from substance use disorders should be included, but that pharmaceutical adverse events that do not involve controlled substances should not be. | |
| Acknowledgements | |
| The authors thank Roxanne Saucier for providing helpful comments on drafts of this manuscript. The authors also thank Kathleen Creppage for sharing findings from an analysis of the literal text of death certificate data. | |
| ND was funded by the Robert Wood Johnson Foundation’s Public Health Law Research program for work on this paper (Grant 69689). No authors have declared any conflicts of interest. | |
| References | |
|
|
Citation: Dasgupta N, Proescholdbell S, Sanford C, Funk MJ, Casteel C, et al. (2013) Defining Controlled Substances Overdose: Should Deaths from Substance use Disorders and Pharmaceutical Adverse Events be included? J Clin Toxicol 3:164. doi: 10.4172/2161-0495.1000164





