The Case for Studying Ibogaine, the Anti-Addiction Drug
Addiction Treatment Articles
Addiction Alternative Treatment
Opioid Addiction Treatment
Addiction Psychopharmacology
Drug War
Drug Prohibition
Addiction Research Articles
Ibogaine Research and Articles
Overview
Originally Published: 10/16/2015
Post Date: 10/17/2015
Source Publication: Click here
Similar Articles: See the similar article
by Yasmin Tayag
Summary/Abstract
Since the 1960s a disparate group of scientists and former drug addicts have been advocating a radical treatment for addiction - a hallucinogen called Ibogaine, derived from an African plant, that in some cases seems to obliterate withdrawal symptoms from heroin, cocaine and alcohol. So why isn't it widely used?
Content
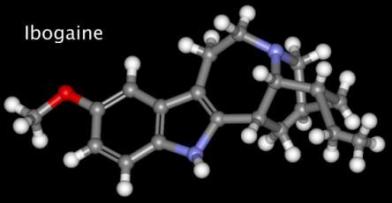
It doesn’t take much digging in the underbrush of the Congo basin to find the iboga plant, an innocuous-looking but hallucinogen-packed shrub that has the potential to revolutionize drug addiction treatment. Still, Ibogaine, the powerful hallucinogen derived from the plant, isn’t as easy to find stateside — it’s classified as a Schedule 1 substance so even academics struggle to get their hands on it. Jonathan Dickinson, director of the Global Ibogaine Therapy Alliance, wants to change that.
“The best thing to say is that ibogaine is an addiction interruptor,” Dickinson toldInverse. After experiencing the drug’s powerful hallucinations, addicts no longer experience cravings. It’s especially useful in drug detox treatment, he says, because of its ability to curb the physical symptoms of withdrawal. These days, most of the evidence for ibogaine’s efficacy comes from outside the U.S. A handful of American studies have taken place, but there is nothing resembling a scientific consensus on best practices for ibogaine use.
Ibogaine, like so many other psychedelics, wasn’t always so maligned. Studies on its potential to help drug addicts were funded by the U.S. National Institute on Drug Abuse as recently as the mid-‘90s, after decades of advocacy by Howard Lotsof, a former heroin addict “cured” by a single dose of ibogaine. Funding was pulled for “various reasons,” says Dickinson, such as issues with cost and intellectual property disputes. Now, as drug addiction tightens its grip on America, interest in ibogaine is appealing again, if not to addicts to the people who work with them.
In a U.S. first, the state of Vermont, struggling to manage its growing heroin problem, drafted a bill earlier this year to allow for the opening of a not-for-profit ibogaine clinic. Ibogaine drug treatment centers already exist in countries like Mexico, and Costa Rica, where Keeping up With the Kardashians star Scott Disick checked in earlier this year. Most centers offer a standard one- to two-week-long treatment, says Dickinson, which begins with a drug dose “stabilization” period followed by tightly controlled ibogaine ingestion and several days of recovery.
The trip itself is unlike any other hallucinogenic experience. “It’s a very powerful psychoactive, says Dickinson. “With drugs like ayuhuasca, there’s not a very pronounced physiological response. But with ibogaine there is. So generally people want to be laid down because, physically, they’re experiencing ataxia, so it’s harder to move their limbs or to walk or have balance.”
Trips often involve a characteristic buzzing sound and a feeling of emotional detachment. “A certain percentage of people also see waking dreams,” says Dickinson. All of the content is incredibly personal, attached to emotional events, and sometimes it appears portrayed in different ways that things actually happened.”
This is not a fun high. Or a particularly safe one. Administered liberally, ibogaine is a deadly poison.
“There are definitely medical risks,” says Dickinson, “but the risks are identifiable.” Certain pre-existing heart conditions and low electrolyte levels are red flags. And because it basically resets a person’s tolerance for opiates, the few users that do relapse are at risk of dying, especially if they take their “usual” dose.
These hazards are simply more reasons why more research is needed, says Dickinson. Ibogaine’s benefits are simply too good to ignore, especially if the risks can be controlled for.
“The reality is that there is nothing else that has come anywhere close or has so many of the qualities in one medicine or in one practice that is able to address all of these different levels of addiction, and that’s what it is.” says Dickinson. “I think that, eventually it will be obvious.”





